I’ve been wondering: Will the 21st Century Cures Act Final Rule change how doctors document? Recently Skeptical Scalpel (surgeon, writer and senior member of the Twitter intelligentsia) shared the experience of a family member who was worried about her cervical MRI report:
My 38 year old non-medical daughter just got the results of her cervical spine MRI online. She was concerned about the biapical scarring. I assured her the radiologist was just being thorough.
(As background, the release of reports to patients is part of a new law called the 21st Century Cures Interoperability & Information Blocking Rule. It kicks in to action this week. Read more in the link. And from here on I’ll call it the ‘Final Rule.’)
In response to Skeptical Scalpel, Penn radiologist Dr. Surabh Jha wondered if this was a problem of patients seeing their reports or a problem of the documentation we’ve grown up with:
To be clear, the issue with reporting clinically irrelevant incidental findings isn’t just that patients read the report & can get worried. It’s why report irrelevant stuff in the 1st place? (apart from demonstrating your mastery of anatomy)
I remember early on it was suggested that the Cures Rule wouldn’t change how doctors need to document. We would just continue to do what we’ve always done.
The Final Rule will change how health professionals document
I suspect that we won’t continue to do what we’ve always done. And over time, the Final Rule will change how doctors document. I’m not judging whether this is good or bad.
This brief exchange on Twitter reflects the kind of conversations that are beginning to happen around medical record transparency. The final rule will force us to confront some of the things that we’ve always done.
As an example, I’ve been struggling with how I use the term anorexia in my charting:
I use the term anorexia all the time to describe loss of appetite in children and babies. And nearly every time it leads to confusion. Then I have to explain the difference between a symptom and a neuropsychiatric diagnosis. Every time I do this I think to myself that I probably should stop doing it. Because the effort to explain the difference isn’t worth the time to try to correct it.
So here’s a question: Were early open notes champions correct when they said I wouldn’t have to change how I document? Absolutely. Am I going to continue to bicker with patients over an obviously confusing word? Absolutely not.
It’s the difference between what we’re required to do and what we will do. And because of this and other examples I’ve begun to change how I document.
We never know how a technology will impact society
Greater transparency and patient agency will be part of the fabric of healthcare going forward. And the best thing we can do professionally is to openly discuss the changing purpose of medical documentation in the context of this cultural shift. As profession under redefinition, partnering with our patients in this mission is a great way for physicians to define themselves.
Joi Ito suggested in Whiplash, The truth is that a technology means nothing, in and of itself…. What technology actually does, the real impact it will have on society, is often what we least expect.
No one can predict how the open note experiment will turn out. But health professionals and their patients are in a great position to help shape and steer our direction.
And creating the future rather than guessing where it might take us is the best approach.
If you like Will the Final Rule Change How Doctors Document you can check out other Cures Rule posts. You can find them in the Final Rule archive. Every post here has tags way at the bottom that will help you navigate the site for related reading. The EHR archive is also interesting.
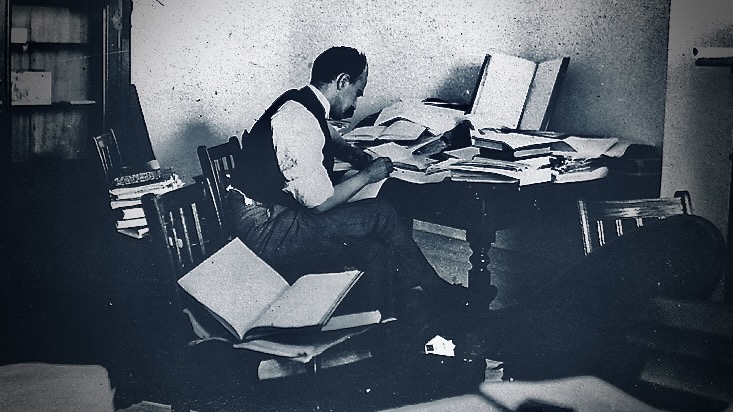
Image: William Osler writing at the Johns Hopkins Hospital